In 2025, Canada has found itself at the center of a troubling measles outbreak, with over 3,800 confirmed cases, primarily affecting children and infants. This figure is strikingly higher than the number of cases in the United States, despite Canada’s smaller population. Alberta has become the epicenter of this outbreak, raising critical questions about vaccine hesitancy and the effectiveness of public health measures in controlling the virus.
The case of four-month-old Kimie Birch from Alberta exemplifies the current crisis. Initially assuming her daughter's fever and rash were from a vaccine reaction, her grandmother promptly identified the illness as measles—a diagnosis confirmed by lab tests. Such unforeseen cases have alarmed health officials, as Canada had not seen measles in such numbers since it was declared eliminated in 1998.
Alberta's measles infection rate is the highest per capita in North America, a statistic that has made Canada the only Western nation on the CDC’s top ten list of countries facing significant measles outbreaks. The outbreak was exacerbated by a recent large gathering of low-vaccination-rate Mennonites in New Brunswick, with the illness rapidly spreading within similar communities in Ontario.
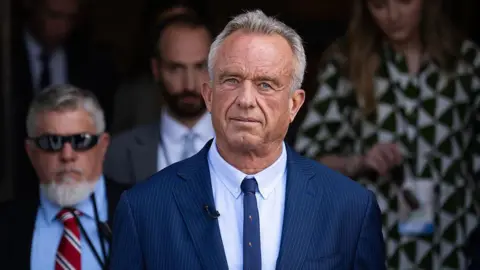
Dr. Maxwell Smith, a public health fellow at Western University, emphasized that various factors contribute to the ongoing outbreak in Canada, noting the absence of a notable anti-vaccine figure akin to Robert F. Kennedy Jr. in the U.S. He pointed out, however, that vaccine hesitancy has increased since the onset of the COVID-19 pandemic, leading fewer parents to prioritize routine immunizations.
In Canada, vaccine uptake has notably declined, particularly among Low German-speaking Mennonites, many of whom adhere to cultural beliefs that discourage vaccinations. This demographic disparity highlights a crucial communication gap between health authorities and particular community groups, and mistrust towards mainstream healthcare can further complicate public health messaging.
Health officials in Alberta have reported a slowdown in new measles cases recently, as vaccination rates have seen a slight increase, particularly following an adjustment in vaccine eligibility. Yet the long-term implications of the outbreak remain a concern, especially with hesitancy around routine immunizations persisting in some communities.
Experts agree that the key to preventing further outbreaks lies in improving vaccination rates and dispelling misinformation about vaccines. They stress the need for continuous community engagement and better outreach to underserved populations to combat the rise in vaccine hesitancy that has only been aggravated by the pandemic.
As Kimie's case unfolds, the frustrations of concerned parents like Morgan Birch highlight the urgency of addressing the ongoing challenges in public health. "My four-month-old shouldn’t have gotten measles in 2025," she lamented, urging others to heed public health guidelines for the benefit of community immunity and the protection of vulnerable individuals.