The study highlights the severe impact of antimicrobial resistance (AMR) on child mortality, reporting over three million deaths due to infections that are no longer treatable with standard antibiotics. Experts warn of a significant rise in AMR-related cases, exacerbated by increased antibiotic use and the lingering effects of the Covid pandemic.
Alarming Rise in Child Mortality Linked to Antibiotic Resistance

Alarming Rise in Child Mortality Linked to Antibiotic Resistance
A recent study reveals that over three million child deaths in 2022 were attributed to drug-resistant infections, emphasizing a growing public health crisis, especially in Africa and South East Asia.
Article text:
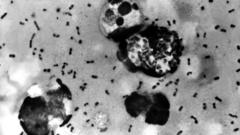
A troubling new study indicates that more than three million children globally succumbed to infections linked to antibiotic resistance in 2022, marking a significant public health crisis that disproportionately affects regions like Africa and South East Asia. The findings underscore the escalating threat of antimicrobial resistance (AMR), a phenomenon where bacteria evolve to resist the effects of commonly used antibiotics.
Researchers, including Dr. Yanhong Jessika Hu from the Murdoch Children's Research Institute and Professor Herb Harwell from the Clinton Health Access Initiative, utilized data from the World Health Organization (WHO) and the World Bank to compile their analysis. They found a worrying increase of over tenfold in AMR-related infections among children in just three years, a trend believed to be exacerbated by the Covid pandemic's effects on healthcare practices.
Antibiotics, essential for treating many bacterial infections ranging from skin diseases to more complex ailments like pneumonia, have seen an inappropriate and overabundant usage. The study found that the rising use of "watch antibiotics," which have a high potential for developing resistance, surged by 160% in South East Asia and 126% in Africa from 2019 to 2021. Concurrently, the usage of "reserve antibiotics"—the last line of defense against severe infections—rose by 45% in South East Asia and 125% in Africa during the same period.
The researchers warn that should bacteria continue to adapt against existing antibiotics, medical practitioners may soon face a grim future with limited treatment options for multidrug-resistant infections. At an upcoming presentation at the Congress of the European Society of Clinical Microbiology and Infectious Diseases in Vienna, Professor Harwell emphasized that AMR is a global issue affecting all demographics, specifically highlighting its devastating impact on children.
While the WHO has classified AMR as one of the most critical global health threats, solutions are not straightforward. According to Professor Harwell, addressing the issue requires a multifaceted approach that spans various medical practices and societal behaviors. Enhanced immunization, water sanitation, and hygiene improvements are critical in preventing infections that could lead to resistance.
Dr. Lindsey Edwards, a senior microbiology lecturer at King's College London, echoed the urgency of new findings, urging global health leaders to take immediate and strong action. Without intervention, the ongoing rise of AMR could reverse decades of progress made in reducing child mortality rates, particularly in already vulnerable populations. As antibiotic usage is projected to increase, it is crucial to ensure that these medications are utilized judiciously and effectively across medical environments.
A troubling new study indicates that more than three million children globally succumbed to infections linked to antibiotic resistance in 2022, marking a significant public health crisis that disproportionately affects regions like Africa and South East Asia. The findings underscore the escalating threat of antimicrobial resistance (AMR), a phenomenon where bacteria evolve to resist the effects of commonly used antibiotics.
Researchers, including Dr. Yanhong Jessika Hu from the Murdoch Children's Research Institute and Professor Herb Harwell from the Clinton Health Access Initiative, utilized data from the World Health Organization (WHO) and the World Bank to compile their analysis. They found a worrying increase of over tenfold in AMR-related infections among children in just three years, a trend believed to be exacerbated by the Covid pandemic's effects on healthcare practices.
Antibiotics, essential for treating many bacterial infections ranging from skin diseases to more complex ailments like pneumonia, have seen an inappropriate and overabundant usage. The study found that the rising use of "watch antibiotics," which have a high potential for developing resistance, surged by 160% in South East Asia and 126% in Africa from 2019 to 2021. Concurrently, the usage of "reserve antibiotics"—the last line of defense against severe infections—rose by 45% in South East Asia and 125% in Africa during the same period.
The researchers warn that should bacteria continue to adapt against existing antibiotics, medical practitioners may soon face a grim future with limited treatment options for multidrug-resistant infections. At an upcoming presentation at the Congress of the European Society of Clinical Microbiology and Infectious Diseases in Vienna, Professor Harwell emphasized that AMR is a global issue affecting all demographics, specifically highlighting its devastating impact on children.
While the WHO has classified AMR as one of the most critical global health threats, solutions are not straightforward. According to Professor Harwell, addressing the issue requires a multifaceted approach that spans various medical practices and societal behaviors. Enhanced immunization, water sanitation, and hygiene improvements are critical in preventing infections that could lead to resistance.
Dr. Lindsey Edwards, a senior microbiology lecturer at King's College London, echoed the urgency of new findings, urging global health leaders to take immediate and strong action. Without intervention, the ongoing rise of AMR could reverse decades of progress made in reducing child mortality rates, particularly in already vulnerable populations. As antibiotic usage is projected to increase, it is crucial to ensure that these medications are utilized judiciously and effectively across medical environments.