NEW YORK (AP) — Enhanced tax credits that significantly reduced the cost of health insurance for a vast majority of Affordable Care Act enrollees expired overnight, resulting in higher health costs for millions of Americans at the beginning of the new year.
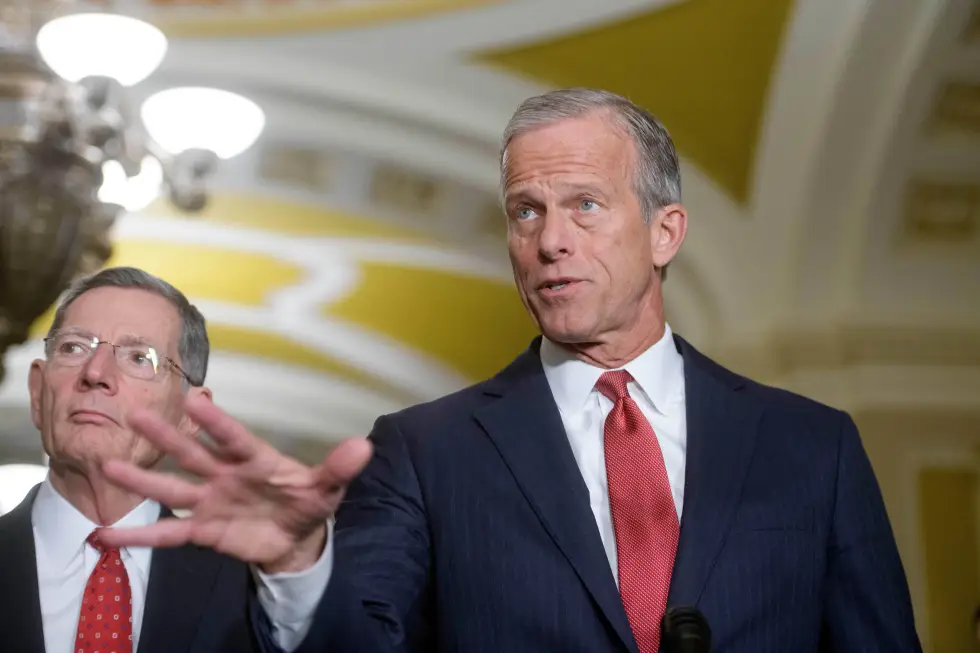
Democratic leaders forced a 43-day government shutdown over this healthcare funding issue, while moderate Republicans called for a solution in hopes of preserving their political ambitions for 2026. However, their efforts were in vain as the tax credits expired without a resolution. A House vote is anticipated in January, yet its success remains uncertain.
This change affects a wide range of Americans who obtain health insurance outside of employer-sponsored coverage and do not qualify for Medicaid or Medicare—impacting self-employed individuals, small business owners, farmers, and ranchers.
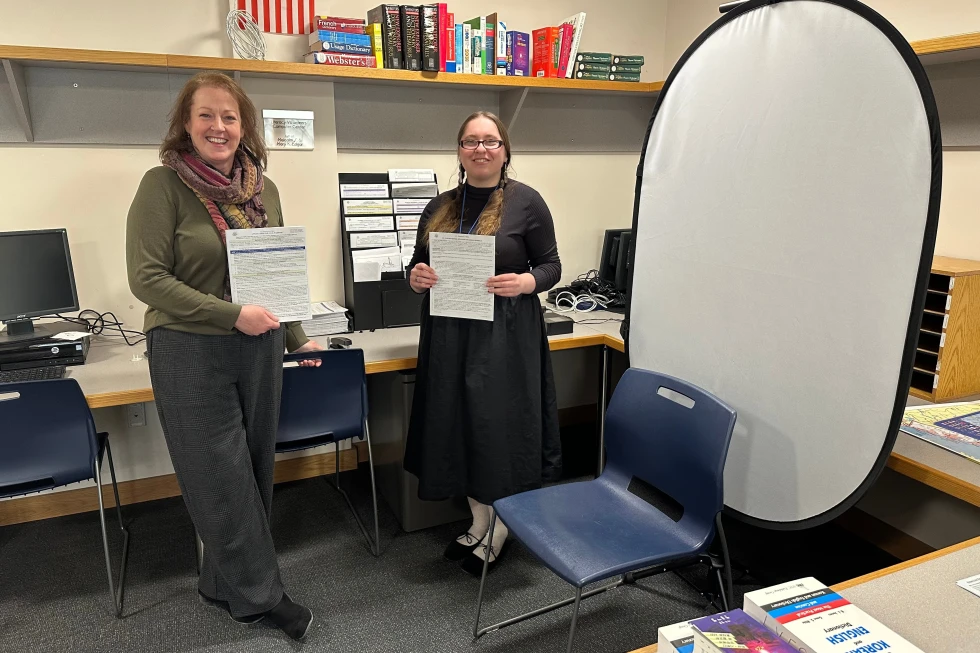
As the country enters a high-stakes midterm election year, maintaining the affordability of health care is a primary concern for many voters. Katelin Provost, a 37-year-old single mother, expressed her frustration, stating, “It really bothers me that the middle class has moved from a squeeze to a full suffocation...I’m incredibly disappointed.”
Some Families Grapple with Costs Doubling or Tripling
The expired subsidies, initially provided as a temporary measure due to COVID-19 in 2021, had been extended by Democrats until 2026. With these subsidies, lower-income enrollees enjoyed little to no premiums, while high-income individuals paid a maximum of 8.5% of their income.
On average, over 20 million subsidized enrollees are facing a premium hike of 114% in 2026, according to an analysis by the health care research nonprofit, KFF. Some enrollees, like Stan Clawson, a freelance filmmaker from Salt Lake City, report significant increases in their premiums. Clawson’s monthly cost jumped from just under $350 to nearly $500, while Provost’s premium surged from $85 to approximately $750.
Enrollment Effects Remain to be Seen
Health analysts are predicting that the expiration of subsidies will drive many of the 24 million total Affordable Care Act enrollees, particularly the younger and healthier individuals, to drop their health insurance coverage altogether.
An analysis by the Urban Institute and the Commonwealth Fund projected that around 4.8 million Americans might lose coverage if subsidies are not reinstated. Currently, consumers have until January 15 to choose or modify plans, so final enrollment numbers are yet to be determined.
Months of Discussion, No Relief Yet
Following massive cuts in federal health care and food assistance, Democrats have persistently advocated for the extension of subsidies. However, a Senate vote in December resulted in the rejection of two partisan health care bills—one proposed by Democrats for a three-year extension and the other a Republican alternative focusing on health savings accounts.
Despite actions from a few centrist Republicans collaborating with Democrats to propose a vote for the extension, previous rejections in the Senate throw its future into uncertainty. Many Americans are voicing frustration, claiming that their struggles with soaring health costs are not being understood by lawmakers.
The call for the restoration of subsidies is coupled with a demand for broader reforms aimed at making health care genuinely affordable for all citizens. Chad Bruns, a 58-year-old Affordable Care Act enrollee, summarized the sentiment: “Both Republicans and Democrats have been saying for years, oh, we need to fix it. Then do it.”